I am allergic to routine. The mere mention of the word ‘schedule’ makes me nervous. I thrive on procrastination, such as writing a chapter or manuscript when the timing is right for me instead of by the calendar. While my fly-by-night timing sometimes worries others, I know how I work best; under pressure I always meet a deadline.
But what happens when life itself becomes a tremendous pressure under the constant burden of illness or caregiving? For me it is too much and routine becomes my salve.
Recently, a family member was in ICU. It was scary. I wanted to meet with the doctor on each of his rounds. I wanted to make sure my loved one was getting the right meds, not being subjected to unnecessary tests, and receiving the best care possible. I also wanted to make sure I got the rest and food I needed to stay healthy, especially given my rickety immune system, stress load, and exposure to hospital germs.
Each night I left the hospital around 10 pm. I made sure to grab a meal with lots of vegetables and protein. By 11 pm I popped a small dose of xanax, reserved for anxiety provoking times such as these. And though I am not a fan of David Sedaris, I found a copy of one of his books on a shelf in my uncle’s apartment and read it every night as I fell asleep tucked into the living room sofa. His writing felt like an NPR hipster version of Chicken Soup for the Soul. His mildly entertaining stories and obnoxiously irritating points of view lulled me into the sleep I desparately needed to face the next day. I made sure to read a page every single night.
Living with an acute medical condition, be it your young adult cancer or the flare of another illness, involves navigating the fear of the unknown. The desire to have stability, a knowable schedule, and predictable routine makes perfect sense. To exert some modicum of control of our out of control lives is sometimes the best medicine of all. (Note: This post was written in the comfort of my bed five days before my house move and I have not yet begun packing boxes.)
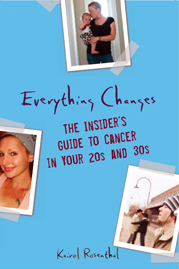
![]()
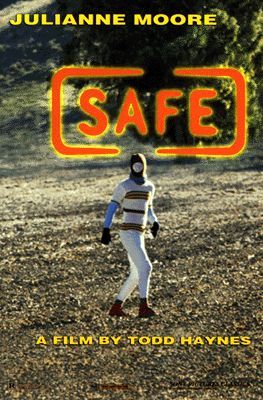
![]()




 “Everything Changes is, without doubt, the most forthright, emotionally sophisticated, and plain-old valuable book of its kind I've seen.”
“Everything Changes is, without doubt, the most forthright, emotionally sophisticated, and plain-old valuable book of its kind I've seen.”