
I’m disturbed that in recent conversation about breast cancer guidelines, I’ve not heard anybody asking the question: ‘What is the most effective way to lower breast cancer mortality rates in young women?’
Prior to this announcement, I’ve spoken with staffers from key organizations serving young women with BC (breast cancer). They told me they’ve never seen studies on whether breast self exams (BSE) lower mortality rates in young women. I’ve read articles in which policy analysts and scientists agree this needs to be studied.
Cancer is terrifying and it is down right frightening to have BSEs diminished as a guideline when they are the one thing we have come to think of as a hopeful solution for young women. But instead of defending a tool about which we have little scientific information, why don’t we get motivated about researching what will save our lives?
I’ve heard tons of stories over the years about young women who’ve found their BC themselves and use this as justification in favor of BSE. We do know that across every age group the majority of BC is first found by women touching their own bodies accidentally or intentionally. Nobody is debating this fact. However there is a world of difference between the two questions of: “Do women find lumps when they do BSE?” and “Does doing BSE lower the mortality rate in young women age 15-39?”
Stories are motivation to find answers, but they are not the answers themselves. The reason we draft legislation and raise money with walk-a-thons and pink ribbons is to fund smart science to help us make the most effective choices about preventing, detecting, and treating BC in young women. I wish the $45 million in Representative Wasserman’s EARLY ACT was directed towards investigating how to best lower mortality rates in young women with BC. Show me a piece of evidence saying that BSE in young adults lowers the mortality rates of 15 - 39 year olds, and that the benefits of this outweigh the harms, and I think we will have hit the jackpot on what we need to do to take care of our generation. Until then, as a community we need to demand that young women be taken seriously, and that government dollars be spent on researching our diseases so we can find the most EFFECTIVE ways to save lives.
Cathy Bueti, a breast cancer survivor and author of Breastless in the City says:
“Although I found my lump it was not from doing a monthly BSE. I never consistently did them. Even today I only get thorough breast exams when I see my doctors twice a year. If I did BSE I would be on the phone every month in a panic with the doctor. Young adults have crazy hormones that can cause frequent changes in breast tissue. BSE can lead to unnecessary biopsy and is not going to increase survival rates in young adults. I was told the lump I found most likely was growing for 10 years so it did not ensure early detection in my case. However, I do believe it is important to stay familiar with your breasts so if you do find something that was never there before you can followup on it.”
As patients it is our obligation to know about breast cancer guidelines from scientific perspectives in addition to our own stories. Here are some important links. Read up!
U.S. Preventative Services Task Force (USPSTF) - These are the folks who issued the guidelines and this link has their research and rationale.
National Breast Cancer Coalition Fund - These folks are an umbrella organization for a lot of other familiar cancer organizations. This link takes you to a page where they discuss the needs and concerns about young women and breast cancer funding, research, and prevention.
Breast Cancer Action - These are some of the coolest gals in the breast cancer world. This link talks about their take on mammograms in women age 40-49. Yep, some of us in the YA cancer community are getting close 40!
Let me know what you think about whether young women’s voices have been included in this conversation. Do you think we can move beyond anecdotal stories about young women with breast cancer and start investing in evidence based studies about how to reduce our mortality rates?
![]()
![]()
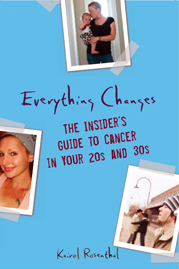
 “Everything Changes is, without doubt, the most forthright, emotionally sophisticated, and plain-old valuable book of its kind I've seen.”
“Everything Changes is, without doubt, the most forthright, emotionally sophisticated, and plain-old valuable book of its kind I've seen.”












November 20th, 2009 at 11:42 AM
Kairol,
It’s funny that you finally addressed this because I just finally addressed it last night. I think there are a variety of things to address here and I’m certainly not going to take up all of your space after your interesting post.
I would like to address the fallacy of breast cancer in younger women being anecdotal. Somewhere between 20 and 25 percent of the women in the U.S. who are diagnosed with breast cancer are under age 49. That is thousands of women.
While I agree that mammography may not be the best tool we have until we have something else we don’t have a lot of options.
By the way there is a really interesting story in the New York Times talking with the doctors who made up the committee that came up with the suggestions and how shocked they are that it has been taken negatively. Apparently they have not been working in the world that the rest of us live in.
Happy Thanksgiving! Kate
November 20th, 2009 at 1:03 PM
Thanks for the great post. I think there are two issues here that we need to come to grips with.
First, medicine works when it is based on science and evidence, not anecdotal stories. Whether an individual thinks that a specific treatment helped them should be largely irrelevant to establishing medical guidelines because: (a) they may be wrong, (b) there may be better treatments that can be pursued, or (c) the treatment may have other side effects or consequences that outweigh any benefit is might provide. Instead of relying on anecdotal stories from individuals, therefore, medicine focuses on wide ranging scientific studies that evaluate the impact of specific treatment on health outcomes, life expectancy, recovery rates, etc. of populations in order to determine whether particular treatments are worthwhile, useless, or perhaps even harmful.
The Task Force has looked at the evidence and concluded that screening for women under 50 is, on balance, not worthwhile. In fact, it is harmful because it leads to unnecessary biopsies that end up making it harder to detect cancer later on. The Task Force concluded that that negative impact and others of screening under 50 more than outweigh the benefits. If people have scientific evidence to the contrary, then that should be evaluated. The objections I have seen, however, seem to be purely anecdotal persoanl stories. While I understand the emotional pull of such stories, the evidence shows that basing medical guidelines on such stories would actually be harmful to the goal that we all share.
A second point is that, as much as we don’t like to admit it, in a world of limited resources, a dollar spent promoting one treatment is a dollar that cannot be spent on another treatment. For example, the millions of dollars that we spend promoting screenings and on the screenings, unnecessary biopsies, etc., aren’t being spent helping breast cancer patients afford their tamoxifen or providing health insurance to young adults who don’t have it. As the head of ACS has said, the number one thing we could do to increase young adult cancer survival rates would be to make sure young adults have health insurance. The evidence tells us that those things work; so let’s spend our money there rather than on screenings that don’t.
November 20th, 2009 at 4:18 PM
Kairol you bring up many good points in this post. I agree with Moses regarding the objections being purely anecdotal. I think that much of what is happening here is that people are reacting to the recommendations with all of their emotion and fear. I understand all too well how hard it is to not be emotional about cancer. I also think there is alot of misinterpretation of the results due to that increased emotion. But we need to look at this much more objectively and let the research guide us and have more money spent on studies regarding mortality rates in young adults.
Thank you Kairol for including my opinion on BSE in this great piece. For anyone who wants to read more info about my bc story as well as my opinion on the mammography guideline aspect of the recommendations head over to my blog.
http://www.cathybueti.blogspot.com
November 20th, 2009 at 5:07 PM
Kairol, while I see both Kate’s and Moses’s viewpoints, your question, “Do you think we can move beyond anecdotal stories about young women with breast cancer and start investing in evidence based studies about how to reduce our mortality rates?” is the one that keeps echoing in my head. My answer is yes - and that needs to happen not just for breast cancer, or cervical cancer (which took a screening recommendation hit today, too) but for ALL cancers.
We not only CAN move research beyond anecdotal stories about detection and diagnosis - we MUST move to accomplish that research.
I agree that decisions are based on (mostly) facts and science and research. And I submit, with all due respect to the learned members of the USPSTF, that it’s entirely possible that while their research is adequate on its face for the question(s) they considered, they asked the WRONG questions.
The questions are not only whether early screenings prevent death, or even whether they cause harm. Those are important questions, but not the only questions that need to be asked. Researchers need to ask whether early screening actually discovers disease in a lower, more easily treatable stage than screenings at a later age. They need to ask if that number is rising (in several cancers, it is.) They need to ask whether early, non-invasive screenings like BSE, mammograms, and other self-exams, can contribute to a heightened body-awareness that helps people become better and more active, informed participants in their health care. They need to ask if it’s more cost-effective to provide preventative care to the largest population possible or more cost-effective to stick with the current model (spending hundreds of thousands of dollars to fight fires that could have been prevented at lower cost.)
We are mired deep in a US healthcare system which spends exponentially more money on treatments (putting out fires) than it spends on preventing those fires in the first place, than it spends on making routine well-person checks available and affordable. The causes of readily available screening and early detection for any cancer are very close to my heart - as well as other areas of my anatomy.
I was considered high-risk for breast cancer (paternal aunt and 3 of her 4 daughters dx’d with BC before age 40; one cousin dead of recurrent BC by age 50; one of her 4 daughters a prophylactice mastectomy patient.) I was considered high-risk for cervical cancer after an HPV exposure in my late 30s. I was aggressively screened for both BC and cervical cancer - who knew the cancer card I’d draw would be stage IV rectal cancer diagnosis at age 48, two years before the recommended screening age and with a less than 15% 5-yr survival rate?
Preventable, treatable and beatable in the context of five chemo regimens, three surgeries and 5+ years fighting for my life is relevant only in the context of what SHOULD have been done! CRC ain’t so treatable, preventable or beatable when your doc finds an 80% tumor load in your liver.
I’m an anecdote, all right, but I’m an anecdote who’s paid attention to all of the facts and figures. My treatments and surgeries to date have cost over $300K, compared to what it would have cost to give me annual screening colonoscopies from age 40 - $8K, at today’s prices. That’s pretty simple math to do, and to factor by the number of late-stage (III, IV) patients diagnosed with CRC this year. As with breast cancer, THAT is the math that needs to be done. We need to ask THOSE questions about early screening.
And until we have the answers to those un-asked questions about the success of prevention, then I’d much rather deal with a false positive and a biopsy that turns out to be negative. It would be infinitely preferable to the treatment required after late detection of an advanced cancer.
Been there, done that, have the ostomy supplies to prove it. ;)
November 21st, 2009 at 1:48 AM
As a cancer survivor and busty woman, I’d rather only only get cancer once. I’ll be pushing for early mammograms and doing self exams often. I don’t want to ever have to go through what I went through again. One cancer battle is enough.
Hope you’re well!
XO
November 21st, 2009 at 3:26 AM
Kelly, The guidelines state: “The decision to start regular, biennial screening mammography before the age of 50 years should be an individual one and take patient context into account, including the patient’s values regarding specific benefits and harms.” It sounds like you certainly fall into that category of an individual exercising their choice to get mammograms early.
I sure as hell hope that you don’t get it too! I agree - once is enough. Ever since my n-th bout of thyroid cancer, I have been very fearful of getting breast cancer. Don’t know why I’ve picked that one to be freaked out about instead of one of the other cancers I am at high risk for… Here’s to hoping we both stay well. Best, Kairol
November 21st, 2009 at 11:51 AM
Thank you for letting me know that other people are wondering what to do IF the exams we have in place are failing women. What is our “plan B”? I mean besides just IGNORING our boobs until we’re 50.
I found my own lump at 35 - Not doing a BSE, just felt the lump, watched it, I was nursing… it could have been something else, but it was cancer. I was not at risk aside from having boobs: perhaps the biggest risk factor, so I had not had a mammo or screening. But there I was.
We do need to screen earlier to Pat’s point, and save lives AND money in doing so. I had aggressive chemo, surgery & radiation. It was a lot for my body and mind to endure(my kids and family too!).
Research on the cause(s), better screenings, smarter medicine and whole body/life consideration… We should be so much BETTER!
November 21st, 2009 at 2:37 PM
[...] in her blog Everything Changes, Kairol Rosenthal asked, “Do you think we can move beyond anecdotal stories about young women [...]
November 21st, 2009 at 5:08 PM
PAT - Those are great questions you asked, and they in fact have been asked and written about by the USPSTF. I think a lot of people are reading headline news and not taking the time to read the full guidelines, evidence, discussion issues, and further recommendations of the USPSTF. These are all there in the link above.
One piece of great news about breast cancer is that while we have thought all along that all breast cancers are extremely aggressive and gotta catch and treat it early - they have now discovered that many breast cancers are in fact slow growing and some can even go untreated for a life time with no harm to the patient. (I know this is a terrifying thought to most, but as a woman who is living with another kind of slow growing cancer and being medically advised to do a wait and watch program - it does take time to adjust to the mind set of not needing to extinguish the fire with a huge hose immediately.) The next step is to improve detection methods so they will be able to differentiate between these kinds of cancer so we are not unnecessarily tearing apart our bodies and spending billions in the process to do so.
I think we are in a relay now between an old paradigm and a new paradigm for which we do not yet have all the answers of how to treat and proceed. I think this is one reason why the recommendations were so generously written to allow for total flexibility for women to discuss with a healthcare provider and chose what is best for them given their risk factors and values.
(And P.S. - Pat, thanks for your excellent comment on my New York Times post about cancer and brain fog. I just read another comment from a reader who also found your insight and book reference very useful!)
November 21st, 2009 at 8:09 PM
After reading everyone’s posting and what other foundations, organizations, and physicians are saying about changing the guidelines to having a mammogram at 50, I will still feel strongly that until a more effective tool is available to detect early breast cancer in young women that self breast examination are important, and we should not mislead any young women to believe otherwise. While younger women are not in the majority getting diagnosed with breast cancers when they are diagnosed their tumors are often faster growing, therefore close attention must be paid to this demographic. In my lectures to high school and college students, I will continue to urge young women to follow the current standards of examination and detection.
My breast cancer was detected by mammogram, which stated that I had suspicious calcifications. It turned out that I had a multi-focal invasive breast cancer leading to removal of my entire left breast, followed by prophylactically removing my right breast 3 months later. While devastated not having breasts for five years, had I not gone for my routine mammogram beginning at age 30 (I have a strong family history)my cancer would never have been detected. I never had a breast lump. However, the microcalcifications that I had for over 10 years and followed by mammogram was found to be cancer at the age of 45.
I thank you for letting me share my opinion.
Cindy Papale, author of The Empty Cup Runneth Over
November 21st, 2009 at 9:51 PM
I’m still sorting through all of the data, opinions, gut reactions and trying to balance it with my personal anecdote and those of dear ones near and far. Obviously we need to keep researching methods for detecting (and of course curing) BC (and all cancers/disease), especially in young women, but in the end I still find it incomprehensible and completely OUTRAGEOUS that the Task Force recommend against teaching clinical self-exams. I understand that it’s officially still open-ended for individuals to make their own decisions with their doctors but unfortunately not everyone is empowered to do so, and I feel strongly that it’s imperative for body-awareness to be taught and nurtured at all levels of health care. I’m particularly concerned about underserved individuals and communities that don’t have access to health care and body-awareness options. I feel this way about the entire body for general to specific health and wellness issues.
Thanks for this objective and thoughtful response, I appreciate the food for thought. Still chewing.
November 21st, 2009 at 10:18 PM
I’m still sorting through all of the data, opinions, gut reactions and trying to balance it with my personal anecdote and those of dear ones near and far. Obviously we need to keep researching methods for detecting (and of course curing) BC (and all cancers/disease), especially in young women, but in the end I still find it incomprehensible and completely OUTRAGEOUS that the Task Force recommend against teaching clinical self breast-exams. I understand that it’s officially still open-ended for individuals to make their own decisions with their doctors but unfortunately not everyone is empowered to do so, and I feel strongly that it’s imperative for body-awareness to be taught and nurtured at all levels of health care. I’m particularly concerned about underserved individuals and communities that don’t have access to health care and body-awareness options. I feel this way about the entire body for general to specific health and wellness issues.
November 22nd, 2009 at 3:28 PM
I REALLY appreciate the intelligent comments that you are all contributing to this conversation. A few days ago I was going out of my mind over the shallow infighting in the cancer community with so many pseudo-debates online with people blasting each other away with arsenals of anecdotal information that had little to do with science, policy, and smart decision making for the best care of womens health at many decades throughout life. All of the comments above, on the other hand, contribute to a really useful dialogue and I thank you for making this happen.
Prior to these guidelines, I had been doing a lot of reading and research about detection in young women in response to the early act. There is an interesting opinion piece from the L.A. Times authored by Steven Woloshin and Lisa M. Schwartz, who are physicians and professors of medicine at the Center for Medicine and the Media, Dartmouth Institute for Health Policy and Clinical Practice. They are the authors of “Know Your Chances: Understanding Health Statistics.” Here is a link to the piece if you want to read it. http://articles.latimes.com/2009/jul/31/opinion/oe-woloshin31
Through researching my own book, I have come to realize that if I want to be an educated cancer advocate, I should really understand more about statistics. Earning an undergrad degree in choreography, I’ve never been exposed to even a basic statistics class. I’m interested in reading their book. Maybe I can start an online book club and some of us can read it together? Whether we like it or not, all of the guidelines that doctors use to treat our cancers are derived from statistics. The better I understand statistics, the more I can make sense of recommendations and guidelines. Knowledge=power.
November 22nd, 2009 at 5:29 PM
Another problem is distribution of care - Why is it that my mother - who has mid to late stage Alzheimer’s is still getting routine mammograms, but the 30-something woman who helps her during the day (and has no health insurance) had to pony up $600 to have one when she suddenly found herself with breast pain (my dad gave her the money) What would happen if my mom was found to have breast cancer? Would they treat it? probably. Would it enhance her life? Absolutely not. What would happen if her helper finds out she has breast cancer? Will she be treated? Maybe. Maybe not. This doesn’t help her! (It doesn’t even help my mother!)
I find myself wondering - is it more cost effective to deny routine screenings to younger people because finding more of these cancers earlier might actually work out to be more expensive than allowing them to fester longer with quicker mortality since one would receive treatment for a shorter period of time. Does that make any sense?
November 22nd, 2009 at 5:31 PM
I agree with Kairol that there have been many thoughtful comments here. And I understand the emotional difficulty of this issue and the pull that personal experience has.
I would note, however, that the only thing that has been offered here by people opposing the Task Force recommendations is anectodal stories. No one has pointed to any scientific evidence that screening under the age of 50 is beneficial.
There is a great op-ed in the NY Times from a University of Pennsylvania professor detailing the history of breast cancer screening and explaining how we have known since at least 1971 that there is little to no evidence behind screening for women under 50. I found this line especially stunning:
“You need to screen 1,900 women in their 40s for 10 years in order to prevent one death from breast cancer, and in the process you will have generated more than 1,000 false-positive screens and all the overtreatment they entail.”
http://www.nytimes.com/2009/11/20/opinion/20aronowitz.html?pagewanted=2&_r=1&ref=opinion
If we really want to help young adults, let’s focus our advocacy and resources on what we know works - providing health insurance to the uninsured - rather than on screenings that we know do not.