By Kristen Schindler
Cancer has a way of destroying the parts of you that you define yourself by. I felt cancer destroyed my ability to push my body to do great things. I am an athlete, but my treatment for Hodgkin’s Lymphoma sucked away most of my energy. I played softball in college, and have invested years upon years into my athletic career. It took only six months of chemotherapy for my body to lose most of the muscle and endurance I had built up over 12 years.
I had expected to struggle physically while I went through treatment. And I even planned to give my body some time to recover once my treatment had ended. However, I was shocked when three months out of treatment, my energy had not bounced back according to the three month timeline my doctor had given me.
This process of rebuilding muscle, strength, and lung capacity, is anger producing and depressing at times. It is a constant comparison to the pre-cancer me. I am unsure if I will ever be the athlete I was before and I do not have time to train and workout like I did when I was in college. I am terrified that my body will never fully recover from cancer, and my athletic ability is the most glaring indication of that.
I have slowly learned to give myself a break, and relish in my small accomplishments. I still want more, but I am realizing I am in the midst of moving forward. I played softball this summer, and I began to see my old self begin to shine through while I pitched multiple games each weekend. Cancer temporarily took away certain self defining characteristics, but my drive and ambition to be better and push myself is one characteristic that has not been altered.
Were you an athlete or avid exerciser prior to cancer and how has your identity changed since your diagnosis?
![]()
![]()









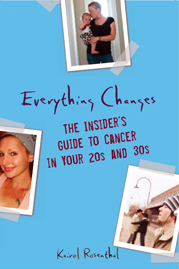
 “Everything Changes is, without doubt, the most forthright, emotionally sophisticated, and plain-old valuable book of its kind I've seen.”
“Everything Changes is, without doubt, the most forthright, emotionally sophisticated, and plain-old valuable book of its kind I've seen.”